- Research
- Open access
- Published:
Strengthening quality in sexual, reproductive, maternal, and newborn health systems in low- and middle-income countries through midwives and facility mentoring: an integrative review
BMC Pregnancy and Childbirth volume 23, Article number: 712 (2023)
Abstract
Background
There is an urgent global call for health systems to strengthen access to quality sexual, reproductive, maternal, newborn and adolescent health, particularly for the most vulnerable. Professional midwives with enabling environments are identified as an important solution. However, a multitude of barriers prevent midwives from fully realizing their potential. Effective interventions to address known barriers and enable midwives and quality sexual, reproductive, maternal, newborn and adolescent health are less well known. This review intends to evaluate the literature on (1) introducing midwives in low- and middle-income countries, and (2) on mentoring as a facilitator to enable midwives and those in midwifery roles to improve sexual, reproductive, maternal, newborn and adolescent health service quality within health systems.
Methods
An integrative systematic literature review was conducted, guided by the Population, Intervention, Comparison, Outcome framework. Articles were reviewed for quality and relevance using the Gough weight-of-evidence framework and themes were identified. A master table categorized articles by Gough score, methodology, country of focus, topic areas, themes, classification of midwives, and mentorship model. The World Health Organization health systems building block framework was applied for data extraction and analysis.
Results
Fifty-three articles were included: 13 were rated as high, 36 as medium, and four as low according to the Gough criteria. Studies that focused on midwives primarily highlighted human resources, governance, and service delivery while those focused on mentoring were more likely to highlight quality services, lifesaving commodities, and health information systems. Midwives whose pre-service education met global standards were found to have more efficacy. The most effective mentoring packages were comprehensive, integrated into existing systems, and involved managers.
Conclusions
Effectively changing sexual, reproductive, maternal, newborn and adolescent health systems is complex. Globally standard midwives and a comprehensive mentoring package show effectiveness in improving service quality and utilization.
Trial registration
The protocol is registered in PROSPERO (CRD42022367657).
Background
There is an urgent global call for increased availability of quality sexual, reproductive, maternal, newborn and adolescent health (SRMNAH) [1]. Literature finds that professional midwives with enabling environments are an effective solution [2,3,4]. The global standard for a midwife is delineated by the International Confederation Midwives (ICM). Although most countries are working toward attaining this standard, wide variation in the definition of midwife within countries remains.
Professional midwives have been found to improve quality in both high- and low-resource settings. However, barriers to practice are also noted [5]. Resistance to quality improvement within health systems is one barrier that can require complex system change to address [6]. In spite of clear World Health Organization (WHO) guidance on SRMNAH, there is a perpetuation of low quality–at times harmful–care in low- and middle- income countries (LMICs) [5,6,7]. The broad sweep of LMICs was chosen to reflect the ubiquitous nature of the problem, however contextual differences between and within countries are acknowledged and warrant further study [7]. The WHO 2021 publication from the Network for Improving Quality of Care for Maternal, Newborn and Child Health (or, the Quality of Care Network) outlines five functions for quality improvement, for LMICs [1]. The first one—onsite support—has been found to be effective in addressing resistance and influencing system change. The provision of onsite support can be key in supporting enabling environments for desired changes, thus it may be needed for midwives to reach their full potential.
Facility mentorship, a type of onsite support, is an increasingly popular approach for enabling quality SRMNAH in LMICs [8, 9]. It comprises both clinical and facility-wide interventions aimed to capacitate and create enabling environments for quality care [10, 11]. Through advocacy, modeling, and problem solving for the needed changes, quality improvements can be achieved.
Mentorship and midwifery have been found to be synergistic as midwives need enabling environments to achieve optimum results, and midwives’ expertise increases the success of mentorship [2, 10, 12, 13]. This review intends to evaluate the bodies of literature on (1) introducing midwives and (2) facility mentoring to better understand facilitators and barriers to implementation of quality, evidence-based SRMNAH care. It aims to provide insight into effective methods of integrating midwives and their related services into health systems [14]. It is hoped that further refinement of our knowledge on this topic will support program efficacy and improve quality of care for the most vulnerable women. The research question was: what is the impact of deploying midwives, and of mentoring midwives, other cadres midwifery roles, managers, and support staff, on providing SRMNAH care in LMICs?
Methods
An integrative systematic literature review was performed with a narrative synthesis approach [15]. The details of the methodology have been published previously [16]. An initial scoping found abundant literature on midwives in high-resource countries and limited literature focused on LMICs. Very few articles from LMICs had a specific focus on the introduction of ICM-standard midwives, or on mentoring to support newly introduced midwives. For the purposes of this review, the term ‘midwife’ included all skilled health workers providing SRMNAH services and was not limited to midwives meeting ICM standards. Facility mentoring was defined as regular visits to health facilities to support providers, staff, faculty, and or managers. Mentors could engage in observation, guidance, feedback, and/or data collection, all with the intention of improving the quality and availability of SRMNAH services. Supplies and equipment as well as infrastructure support were not considered mentoring. An integrative systematic review was chosen as it encouraged the inclusion of diverse articles, thus allowing for a more robust comprehensive review [15, 17].
Inclusion and exclusion criteria
The review was guided by the Population, Intervention, Comparison, Outcome (PICO) framework [18]. Inclusion and exclusion criteria are listed in Table 1. The review included literature from the last 13 years (Jan 2010 to May 2023) that addressed systems strengthening in LMICs through the introduction of midwives, enabling environments for midwives, mentoring, and achieving quality of care. Reviews from the past thirteen years are thought to capture current contexts and issues [19]. Only articles published in English were included.
Information sources
The review was conducted in February of 2023. The literature was searched through Medline, EMBASE, and CINAHL. In addition to the database search, internet searches of published reports and gray literature, and hand searching of relevant reference lists were performed using a snowball approach. References were managed using an EndNote citation manager.
Search strategy
The review was carried out using a priori planned searches. It was inclusive of all literature that addressed the introduction of midwives and/or the use of mentoring to improve SRMNAH in LMICs, including qualitative experiences of those involved. Predetermined key concepts were searched with specific subject headings and the related Medical Subject Headings (MeSH) or thesaurus terms, as shown in Table 2. The search was ConceptTerms1 AND ConceptTerms2 AND ConceptTerms3. Additionally, we conducted a systematic search of relevant gray literature sources using these search terms and key concepts to include gray literature in this review. After identifying relevant gray literature documents, such as government reports, conference proceedings, and institutional repositories, that align with this research topic, we critically assess their quality and relevance to our research question, applying the PICO inclusion and exclusion criteria. Finally, we synthesized the key findings from the selected gray literature sources alongside findings from peer-reviewed literature.
Study selection
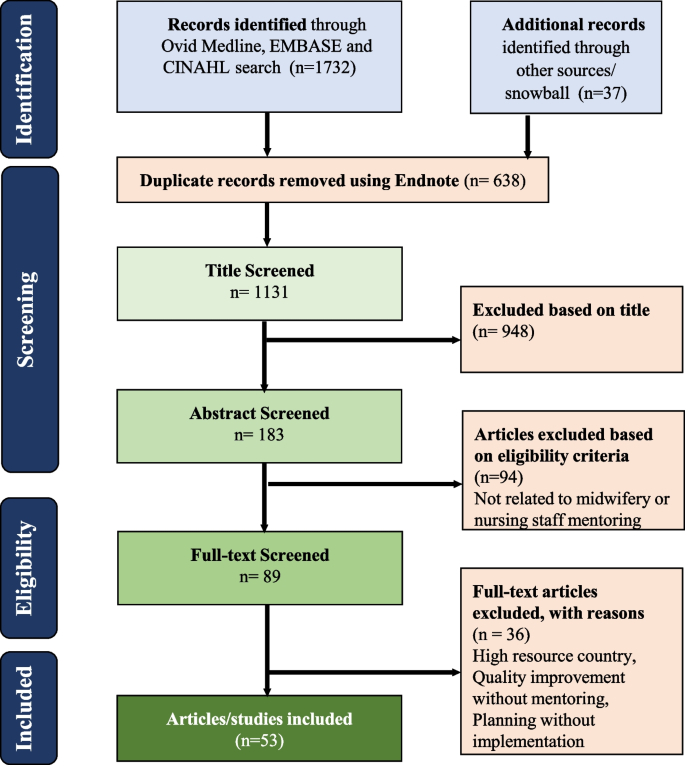
The process of screening and reviewing abstracts and full-text articles based on eligibility criteria is presented in Fig. 1 [20]. After the initial titles were screened, the authors (RA, SBZ, ANJ) screened all abstracts against the inclusion and exclusion criteria. The full texts of all abstracts were then reviewed by the authors (RA, SBZ, ANJ).
Quality assessment
All selected articles were reviewed for quality and relevance. A combined, modified mixed-methods synthesis tool was used with the Gough (2007) weight-of-evidence framework [21]. The Gough tool guides quality evaluation using four themes: coherence and integrity, appropriateness for answering the question, relevance and focus, and overall assessment (Table 3). Using the tool, each theme was given a rating of high, medium, or low. These ratings then combine to form an overall rank. Author RA and SBZ independently reviewed and ranked the articles based on the above criteria, and results from the individual rankings were discussed. In case of discrepancies in rankings, the final decision was taken by the principal author (RA). All articles were included with recognition given their potential strengths and weaknesses.
Data analysis and presentation
As this was an integrative review, there were multiple types of research used. The articles were sorted by research types using five broad categories: 1) project intervention, 2) retrospective country analysis, 3) qualitative process description, 4) literature review, and 5) modeling study. This helped reduce risk of bias by at once evaluating a wide range of studies and distinguishing findings by their research approach.
A health systems building block framework was used to guide data extraction and analysis by the three authors (RA, SBZ and ANJ). Data from the articles were iteratively compared to identify common sub-themes relevant to the research question [17]. The sub-themes were coded and aggregated to identify emerging themes under the existing health system building blocks: national policies and administration, care quality, health-seeking behaviors, experiences and underlying motivators of staff, health outcomes, access to essential medicine, and information systems were identified (Table 4). Although the themes are distinct, they could also be described as steps in a process, tied to and dependent on each other. They are also aspects of the health systems building blocks.
Following theme identification, articles were categorized according to the building blocks. A master table and supplementary tables were created to classify each article according to its Gough score, country of focus, themes, building blocks and methodology. The table also categorized articles according to whether they were inclusive of midwives and or mentoring, if care providers met an international standard for midwives, and how mentoring was defined. To minimize risk of bias in the synthesis of findings, articles involving interventions (methodology type 1) were disaggregated to identify interventions most likely to be transferable. Disaggregation was based on their approaches to measuring outcomes and direction of change. Four outcomes measurement approaches were determined: 1) self-reported or before/after tested knowledge or skills; 2) observed quality improvement at clinical sites; 3) information system health outcome tracking; and 4) facility data on service utilization.
Results
The results analysis is divided into three sections. We provide an overview of key characteristics, rankings and methodological approaches. We then present an analysis of the two main themes (a) midwives and/or both midwives and mentors and (b) mentoring, which emerged from the studies. Finally, we offer a comprehensive synthesis of the specific findings related to midwifery and mentorship according to the health system building blocks approach observed across the included studies.
Fifty-three articles were included in this review (Fig. 1) [22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73]. Tables 5 and 6 at the end of the article display all article data. Among them, 13 were ranked as high, 36 medium, and four low (Table 5). In addition, 18 focused on the introduction of midwives, 29 on mentoring, and six combined midwife introductions with mentoring. Ten articles described midwives meeting a global ICM standard while the others described a range of categories of staff who were called midwives or were providing maternity care. These included nurses, midwives not meeting ICM standards, midwives with unspecified education, general maternity staff (i.e., not midwives), and skilled birth attendants with unspecified education (Table 7, also at end). Across both midwifery and mentoring articles, theme categories yielded overlap, with all articles aligning with multiple themes.
Among the articles focused on midwives and/or both midwives and mentors, seven assessed interventions, seven were retrospective country analyses, five were qualitative process descriptions, four were literature reviews, and one was a modeling study (Table 5). Key barriers were found across articles that limit midwives’ ability to provide quality care [2, 12, 39, 66, 74]. These included policies and work environments that relegated midwives to support roles and constrained their scope and opportunities for growth. For instance, midwives were found to have limited opportunities to attend normal births, and restrictions from managers on providing aspects of evidence-based care, including managing life threatening emergencies. In her integrative review of midwifery programs in LMICs, Schuldt (2019) noted that only one third of midwives were practicing to their full scope [12]. Despite the challenges, all midwives were providing aspects of midwifery care and many midwives were successfully expanding their roles and improving care quality [36, 59, 64, 73]. Evidence-based policy and guidelines, supportive management, mentoring, and continuous professional development all enabled midwives’ performance. Practicing to their full competencies was more likely when midwives met a global standard and when facility mentoring was provided [59, 60, 64, 73].
Of the articles that addressed mentoring (including mentoring of midwives), thirty evaluated mentoring interventions and five were literature reviews. Most mentors were project-based, providing support to government health facilities; some were government employees [23, 36, 40, 44, 45, 61, 62]. Except for one project that used international mentors, all mentors were national nurses, midwives, or doctors and all mentorship was conducted onsite [64, 65]. Mentors largely received pre-mentoring training of up to a week, while some described only existing professional expertise. Three studies described a five week training [23, 31,32,33, 48]. Frequency of mentor visits and mentorship approaches varied across projects. Most mentors conducted from bi-weekly to bi-monthly visits ranging from a total of six facility visits to bi-weekly visits for over 18 months [27, 43, 48, 52]. In two projects, mentors were deployed full time [69, 74]. Most mentoring visits lasted one day and visit frequency was positively correlated with quality improvement [45]. While most mentoring focused on service delivery, three articles described mentoring as part of midwifery education to improve quality of classroom teaching and clinical teaching at practice sites [60, 64,65,66]. Components of mentoring visits included group teaching, case studies, bedside teaching, assessing and advocating for supplies and equipment, establishing and reinforcing data systems, and providing problem solving support [23, 30, 36, 40, 44, 45, 47, 61, 62]. Checklists for mentors to guide their mentoring were mentioned in ten studies [49,50,51, 58, 69]. The mentoring programs that found improvements in outcomes mentored at least twice per month for at least a 3-month duration [49, 51].
The six studies that described introducing midwives in education and practice with mentoring support found additional benefits of mentoring when introducing a new midwifery profession [32,33,34,35,36,37]. This was largely because of improved enabling environments. The benefits of combining mentoring with the deployment/strengthening of midwives include improved quality of care and improved service utilization. One study found statistically significant improvements in use of ANC cards and partographs over what was found with introducing midwives alone [60].
Across all 31 articles that described interventions, none achieved 100% of identified quality improvement goals. Nine articles highlighted gaps in achieving desired goals [37, 38, 41, 43, 46, 47, 69,70,71]. Outcomes measurement approaches with direction of change are delineated in Table 7. Participant self-reported or researcher tested improvements in knowledge or skill, and researcher observed quality improvements were the most common approaches. Twenty-seven and 20 articles respectively showed improvements in outcomes using these approaches. Eleven articles reported improved outcomes using health facility data, eight reported increased service utilization, nine highlighted gaps in achieving desired goals, and one reported no improvement. Most intervention articles included baseline and endline observations and some were retrospective evaluations looking at sustainability. Notably, due to larger numbers of mentorship articles examining interventions, more rigorous outcomes measurement information is available on mentoring than on introducing midwives.
Across all articles, the most common building block themes were governance and leadership, and service delivery, with 31 and 28 articles aligning respectively (Table 6). Eleven or fewer articles aligned with access to essential medicine and supplies, data/ health information systems, finance, and health workforce. Studies examined 23 countries: Afghanistan, Bangladesh, Benin, Botswana, Burkina Faso, Cambodia, Ethiopia, India, Indonesia, Jordan, Kenya, Laos, Morocco, Malawi, Nepal, Pakistan, Peru, Rwanda, South Africa, Sri Lanka, Tanzania, Uganda and Zambia (Table 8) [33, 37, 39,40,41, 43, 44, 47, 52, 58, 62, 64, 65, 69,70,71, 73,74,75]. The following sections discuss the findings in further detail according to the health system building blocks, with midwifery and mentorship specific findings presented separately within each section.
Leadership and governance
The 33 articles that touched on leadership and governance discussed strengths and gaps. They aligned neatly with both the leadership and governance building block and the theme national policies and administration drawn from the review. Thirteen articles looked at the introduction of midwifery, and 18 looked at mentorship interventions. Another two looked at mentorship supporting midwives. Eight were rated high, 22 medium, and three low. The types of articles that addressed leadership and governance included intervention/ program interventions (17), retrospective country analysis (05), qualitative process review (05) and six literature reviews. Most articles on mentoring focused on local-level service delivery governance, including of managerial staff, and systems for overseeing implementation. Midwifery articles more commonly looked at national policies and guidelines. The articles broadly point to evidence-based leadership and governance that reflects ground realities being essential for midwives to practice to their full competencies. Workplace settings that are unsupportive to midwifery, a ground reality, significantly detracted from full scope midwifery and service quality, while supportive workplace settings fostered full scope practice and quality sexual, reproductive, maternal, newborn and adolescent health (SRMNAH) services. Supportive workplace settings typically involved manager engagement through various modes.
Strong leadership and clear global recommendations have helped shape national policies on midwifery and SRMNAH quality improvement [1, 9, 14, 24, 42, 76, 77] [1, 54, 61]. Global and national standards for midwives have brought stakeholders together and are an impetus to support midwifery in spite of competing interests [59]. Political will and multi-stakeholder collaboration were found essential for a quality midwifery profession [61]. Good governance of logistics and infrastructure were also identified as essential, though gaps were highlighted in adequate space for care provision, privacy for respectful care, and commodity availability [54, 56]. Gaps in midwifery leadership were also noted. Lack of leadership by midwives of the midwifery profession may contribute to reduced political will for midwifery care. Country experience shows that professions other than midwives that are positioned as leaders of the midwifery profession sometimes do not fully understand midwives’ expertise and may compete with midwives for maternity care provision roles [12].
Policies that scale up education and deploy midwives closer to communities were found to have a positive impact on service utilization and health outcomes [68]. However, gaps in both of these policy areas were also noted. First, adherence to globally recommended midwifery competencies in education programs is often not abided by in countries [54, 66, 72]. Second, World Health Organization (WHO) workforce guidelines define the number of needed health care workers per population, but not the number of midwives needed [14]. Other gaps related to deployment policy were also identified. For instance, unsupportive workplaces resulted in constraints to optimal midwifery performance in studies in both Pakistan and Bangladesh [11, 28, 74]. In these contexts, midwives either did not perform their duties, or they operated under policies that restricted them from doing so. Governance that did not take into account the inputs needed to create an environment conducive to midwifery within workplace settings was associated with lesser success. One mentoring program that reported no improvement identified restrictive national policies as a barrier [28]. Across articles, few midwives reported supportive workplace settings, and some reported humiliation, including by their direct managers [12, 39, 65, 72]. When managers were not fully involved, resistance to midwives in leadership roles, autonomous practice, and quality improvements in clinical care was found [60, 74, 78].
Conversely, local governance supporting midwife-friendly workplace settings improved midwives’ sense of competence and care quality. Webster et al. (2013) and Schuldt et al. (2020) found that midwives felt competent to provide midwife-led care in supportive workplace settings [29, 59]. Importantly, involving onsite managers to strengthen ownership of midwifery and quality SRMNAH was identified as a priority in twenty-five articles utilizing a range of methods to measure outcomes [30, 36, 60, 74, 78, 79]. Furthermore, support from managers for midwifery care and improved quality was better when on-site mentoring was present [30, 36, 60]. Seven articles found that initiating the well-known WHO quality improvement process, with a focus on SRMNAH, was an effective and easily accepted method of mentoring managers [30, 36, 49, 52, 58, 60, 69, 79]. Taneja et al. (2021) describe initial handholding support and coaching for managers as part of the quality improvement process for SRMNAH in India [79].
Service delivery
Nearly all selected articles—47—addressed service delivery. Of these, 12 included the introduction of midwives, 29 included mentoring, and six included both (Table 7). The themes of care quality, service utilization and health outcomes mapped to the service delivery building block, with 39 articles addressing care quality. Due to their large number, articles addressing service delivery are discussed by theme. Of the service delivery articles, 31 were intervention evaluation, six reported retrospectively on the impact of national programs with a midwifery component (i.e., retrospective country analysis), two were qualitative process reviews, and eight were literature reviews.
Care quality
Among the 39 articles that had a focus on care quality, nine ranked high, 28 medium, and two low. Four included the introduction of midwives, 29 included mentoring, and six included both the introduction of midwives and also mentoring. Gaps in quality education and services were noted in most articles and both introducing ICM-standard midwives as well as mentoring enabled improvements [29, 30, 34, 38, 42, 60, 64].
Studies on introducing midwives reported that ICM-standard midwives improved service quality as defined by WHO maternity care guidelines. Improvements were seen in tertiary medical centers, sub-district hospitals, and non-governmental organization (NGO) supported facilities, as well as in clinical education for nurse, doctor and midwife students [60, 64, 74, 78]. Analysis using logistic regression found that midwives significantly increased the number of women laboring in upright positions, delayed cord clamping, and immediate skin to skin contact after the birth [60, 64].
The large number of mentorship focused studies found that mentorship contributed to quality improvements in midwifery education, comprehensive and respectful SRMNAH services, and emergency obstetric and neonatal care. Studies found gains made in quality education in both classroom and clinical teaching [60, 61, 65, 66]. Midwifery educators identified that online mentoring helped them improve curriculum implementation [65]. Onsite mentoring improved teaching pedagogy, students' access to labs and libraries, and clinical teaching [64]. In addition, quality of care provided at clinical education sites improved after mentoring [60, 61, 64].
Comprehensive and respectful SRMNAH care quality showed improvements with mentoring in studies Afghanistan, Bangladesh, Rwanda, India, Nepal, Jordan, Botswana, Ethiopia, South Africa, Kenya, and Uganda [23, 44, 47, 52, 58, 62, 65, 69,70,71]. An analysis of program data by Save the Children and UNFPA (2021) from 47 mentored health facilities with newly deployed midwives in Bangladesh, found improved respectful communication, partograph use, upright position for birth, and companionship as well as a notable increase in health facilities receiving obstetric emergencies coming from the community [64]. Using observation data, Anderson’s et al. (2022) mixed methods observational study found that midwives in Bangladesh without mentoring made quality improvements, but, with the addition of mentoring, use of ANC cards and partograph increased significantly [60, 64].
Mentoring also contributed to better identification of high-risk pregnancies, improved diagnosis and treatment of STIs, better sterilization and cleanliness practices, and strengthened laboratory capacity to manage pregnancy and newborn-related emergencies in Rwanda [31, 38]. Research in India, South Africa, Uganda, and Rwanda found that mentoring contributed to stronger newborn care services [23, 30, 38, 39]. Despite the many documented benefits of mentoring, there is also evidence of care quality gaps remaining in programs that received mentorship. For example, Tiruneh et al. (2018) found improvements in newborn care in a study in Ethiopia, with the exception of newborn resuscitation [38] and Tripathi (2019) found little improvement in post-partum care and newborn resuscitation in India [35].
Service availability and utilization/ health seeking behaviors
Sixteen articles touched on service availability and/or utilization [22, 24, 34, 38, 42, 50, 64, 73, 74]. Three were ranked high, 11 medium, and two low. Eight were related to introducing midwifery, five assessed mentoring interventions, and three looked at mentors who supported mentors. For the most part, the introduction of midwives was associated with increased SRMNAH service availability and utilization. In a Lancet article, Van Lerberghe et al. (2014) found increased facility births with multi-pronged interventions that included educating and deploying midwives [24]. Vieira et al. (2012) and Speakman et al. (2014) found greater uptake of ANC and skilled birth attendance in studies in Indonesia and Afghanistan [26, 27]. Tasnim et al. (2011) found increased ANC, facility birth, and postnatal care (PNC) following the introduction of ICM-standard midwives in Bangladesh [22]. Another study of ICM-standard midwives in Bangladesh found increases of 27%, 13% and 12% for ANC, facility birth, and PNC respectively [22, 64]. However, other Bangladesh research looking at ICM-standard midwives using a different sample of hospitals found no difference in facility births nine months after a national deployment of ICM-standard midwives [60]. Studies that found gaps in enabling policies and/or workplace settings for midwives showed fewer increased in service utilization [28, 50].
As discussed in the earlier sections, studies on mentorship interventions showed a consistent association between engaging managers in supportive workplace settings and care quality. Related to this, mentorship also influenced service availability and utilization. Two studies led by Anderson et al. (2022) and one led by Save the Children and UNFPA (2021) documented greater availability of cervical cancer screening, postpartum family planning, gender-based violence screening, and post abortion care with mentors supporting new midwives [60, 64, 74]. In research from Ethiopia, Uganda, and India, ANC and facility birth rates in their studies in Ethiopia, Uganda, and India in which mentors supported midwives. Tiruneh et al. (2018) found higher rates of care seeking for obstetric emergencies as service availability improved [38]. Namazzi et al. (2015) and Waiswa et al. (2021) found an increase of more than 20% in sick newborn care visits in Uganda [30, 56]. Stephens et al.’s (2019) study saw a more than doubling of PAC service use including associated family after a mentoring intervention focused on service quality in Tanzania [50].
Health outcomes
Twelve articles reported health outcomes. Three ranked high, seven medium, and two low. Seven included the introduction of midwives and five had a mentoring intervention. Program interventions that were associated with improved health outcomes were thought to be the most likely to be transferable and thus were analyzed more closely to identify research methodology as well as intervention components. Ultimately, the goal of health care is to improve outcomes, and selected studies found improvements in health outcomes associated with midwife deployment [25, 28, 42].
Seven midwifery articles described improved outcomes with the introduction of midwives [24,25,26,27, 29, 43]. All were large national interventions that included many components in addition to midwives, making it difficult to ascribe attribution [24, 26, 43, 49]. One was a multi-country study evaluating the introduction of skilled birth attendants (SBAs). It had mixed results but did find decreased neonatal morbidity in Latin America, the Caribbean and partially for Asia [25]. Vieira et al. (2012), Webster et al. (2013), The World Bank (2013), and Speakman et al. (2014) found significant reductions in maternal mortality in retrospective national analyses of national midwife deployments in five countries [26, 27, 29, 42]. However, analyses of similar programs in India and Pakistan did not reduce maternal mortality [28]. The studies of projects in Indonesia and Bangladesh found that, when midwives were deployed, deaths from obstetric complications, particularly abortion, sepsis, and postpartum hemorrhage, fell over control groups of facilities that did not deploy midwives but rather used doctors and nurses in midwifery roles [22, 60, 64, 74]. Bartlet et al.’s (2014) LIST modeling exercise estimated that under even a modest scale-up, midwifery services including family planning would reduce maternal, fetal, and neonatal deaths by 34% [67].
Neonatal outcomes were inconsistent in a systematic review assessing the protective effect of SBAs on neonatal mortality in nine LMICs [25]. Where SBAs were protective in Latin America, the protection was partial in Asia, and not at all in Africa. An article from Nigeria found that SBA rate was not associated with better neonatal outcomes. Meanwhile, Viera et al. (2012) found a reduction in under 5 mortality in Brazil [26].
Four of the five mentoring articles reported improved health outcomes. All were mentoring ICM-standard nurse-midwives or midwives [52, 56, 57, 69]. In addition, all had comprehensive facility mentoring programs that visited at least twice monthly for at least three months, included managers, and strengthened data collection systems. Three were inclusive of training, two with simulation, and three provided medicine and equipment. However, certain outcomes did not improve. One study from Uganda notes declining MMR in project districts[56]. Studies from Uganda, Rwanda, and South Africa identify declining trends for stillbirths and or neonatal deaths[30, 45]. In Uganda neonatal death was reduced from 30.1 to 19.6 deaths/1,000 live births. In addition, declines in neonatal morbidity including, asphyxia were found in Kenya, Uganda, and South Africa [57].
Health workforce
Like care quality, studies that addressed workforce comprised a relatively even split between focusing on introducing midwives and implementing mentorship programs. Seven examined midwife introduction and five mentorship; one addressed midwifery combined with mentorship. They were largely good quality with six and five rated as high and medium respectively. Two were given a low rating. The theme experiences of midwives and their support staff most aligned with the health workforce building block and is discussed in this section. [28,29,30, 60, 66]. Research quality varied and it was not always possible to discern whether attitudes were presumed or directly expressed.
Reports on midwives and other maternity staff and managers highlighted both positive and negative experiences. Some articles talked about midwives’ dissatisfaction with their workplace or feasibility to implement what was expected of them. Three studies reported midwives’ discomfort with their deployment status and the impact of those discomforts on their performance. Speakman et al. (2014) found that midwives in Afghanistan were less willing to work in military-controlled areas, stating fears about security and resistance from family [27]. Mumtaz et al. (2015) reported that newly deployed midwives in Pakistan stated difficulty in setting up private midwifery practices within rural communities, as distances made traveling prohibitive, particularly at night [28]. One study published in the Canadian Medical Association noted midwives' preference for positions with higher pay and not always choosing to serve the poorest [29].
Anderson et al.’s (2022) study found that midwives expressed un-elicited pride regarding their profession, particularly where midwives were enabled through mentoring. In this and other studies, midwives expressed a desire for professional autonomy, respect, and for midwifery to be a distinct profession [27, 60, 65]. In two of these studies, newly deployed ICM-standard midwives in Bangladesh expressed confidence and competence to provide quality SRMNAH services, while also expressing frustration with imposed limitations by managers and other maternity staff. Anderson et al. (2022) also found that some managers and nurses felt that midwives did not have the competence to practice autonomously or manage emergencies. Managers expressed those nurses’ felt competition with midwives and that this competition led to nurses questioning midwives’ competence.
Many articles on mentoring shared providers’, faculty’s, mentors’, and administrators’ appreciation of and knowledge gained from mentoring [52, 56, 57, 69]. Mentees in the studies in Bangladesh, Uganda, and Karnataka expressed having increased confidence and feeling happy with the mentorship and what they had learned [30, 60, 66]. Studies in India and Bangladesh observed that mentoring contributed to better teamwork among maternity staff [60]. In Laos, a mentorship program designed for newly deployed inexperienced midwives was found to be well-received by hospital administrators [31, 40]. Overall, mentoring led to positive experiences for maternity staff and maternity staff and managers were more appreciative of midwives when there was mentoring [60].
Access to essential medicine and supplies
While it was not one of the initial themes identified, eleven articles mentioned improving essential medicines [23, 31,32,33, 39, 44, 45, 49, 52, 64, 68]. All examined mentoring and two discussed program interventions that introduced midwives with mentorship. Four were rated high and seven medium. Anderson et al. (2022) and Save the Children and UNFPA (2021) addressed the impact of introducing midwives on medicine availability in their studies in Bangladesh [60, 64]. In both of these articles, midwives alone did not make an impact on medicine availability. However, with mentoring, medicines became more available [60, 64]. In an example from Anderson et al.’s (2022) observational study, oxytocin and MgSo4 availability was as low as 13% in facilities without midwives or mentorship, and as high as 81% in facilities with midwives and mentors [60]. Articles on mentoring interventions in India, South Africa, Rwanda and Uganda also reported a positive impact of mentoring on availability of essential medicines [23, 30, 31, 39, 44, 45, 49, 52, 64]. Improvements may be a result of capacitating health workers and supply chain staff to activate supply chain systems. They may also be the result of improved confidence of health care providers and managers to provide the needed care and thus ensure supplies.
Data systems
Ten articles reported on data or health information systems, also not an initial theme [23, 30,31,32, 36, 37, 39, 51, 56, 58, 69]. All ten looked at mentoring and reported strengthening data systems to track SRMNAH services. Articles emphasized the importance of using data to track implementation, such as a detailed clinical record which is sometimes called a case sheet [23, 31, 32, 36, 37, 56]. Namazzi et al. (2015) describes assessing the status of the patient charts and registers at baseline and then having the MOH approve file folders for inpatients to standardize record-keeping and to facilitate data availability [30]. The introduction of individual client records allows for more detailed monitoring of patient care. Synergizing SRMNAH with existing quality improvement systems included increased emphasis on and of utilization of SRMNAH data for program monitoring [36]. Taneja from India describes involving government stakeholders to build on existing data systems to ensure data-based decision making within SRMNAH [79].
Health financing
Eight articles included a focus on health financing, which overlapped with the theme national policies and administration [23, 24, 26,27,28,29, 43, 68], Five related to midwifery and three included mentoring. Cost effective programs are essential in low-resource settings as even if projects are effective, sustainability is dependent on resources [56]. This review found that programs to introduce midwives and those supporting mentorship can be accomplished with minimal expenditure [23, 31]. Midwifery models were noted to be significantly less costly then obstetrician led models for care [67]. Bartlett et al. (2014) found that midwifery models were almost twice as cost-effective as obstetric models ($2,200 versus $4,200 per death averted). The introduction of midwives as well as mentoring can also be implemented within existing government systems using government employees and thus add very little additional cost. However, mentoring projects using government staff sometimes encountered constraints on availability of mentors’ time. Yet, one of the most effective mentoring projects that impacted health was implemented through existing government staff [10]. Even if project mentors are used, research from India found mentoring only increased cost by $5.60 per pregnant woman, or around $460,000 annually for eight districts, making it a cost effective intervention [23].
Discussion
This review underscores the significance of adhering to a global midwife definition and emphasizes the importance of onsite support in creating enabling environments. The health systems building blocks served as an effective framework for interpreting the results through the lenses of its various pillars. It is worth noting that the articles focusing on midwifery, as opposed to mentorship, had fewer intervention studies and more retrospective national and qualitative process research. This research gap limits our understanding of the effective steps required for implementation of successful midwifery programs, as has been mentioned in earlier literature [5]. Among the themes explored in the midwifery literature, governance and leadership emerged as a critical first step. However, there is a pressing need for implementation research that delves into the process and impact of introducing midwives in LMICs. Drawing insights from the literature on mentoring and quality improvement holds potential for guiding countries in devising effective midwife deployment strategies [42].
One notable gap identified in this review pertains to midwife leadership [59]. The significance of midwives leading the midwifery profession has been highlighted in other literature as well [80]. Competition between professions involved in maternal health—midwifery, medicine, and nursing—for leadership roles is recognized as a hindrance to midwives fully realizing their potential. Concerns associated with non-midwives leading midwives include potential conflicting self-interest and gaps in understanding. Midwives possess unique expertise in providing quality routine SRMNAH care to essentially healthy women and newborns. If midwives are not self-governing, their distinctive vision may not be fully implemented. Therefore, more research is needed to identify best practices for promoting midwives into leadership positions.
Although the majority of articles included in this review did not explicitly address the importance of globally standard midwives, those that did emphasized its priority. The literature on skilled birth attendants emphasizes the significance of expert maternity care providers and reiterates the components of globally standard midwives. However, gaps persist in countries' adherence to global recommendations [77, 81]. Additionally, the scope of practice for midwives includes comprehensive sexual and reproductive health, as called for in the sustainable development goals. However, many non-standard midwives lack this expertise. Articles reporting changes in health outcomes consistently involved globally standard midwives, while those reporting no change often featured non-standard providers lacking basic knowledge. Further research is required to examine the impact and decision-making processes regarding the perpetuation of non-standard midwives within countries.
While all midwives provide aspects of midwifery care, this review identified significant gaps in their ability to perform to their full competencies. These gaps inevitably limit the contributions midwives can make. Enabling midwives to practice fully is particularly urgent in managing life-saving emergencies and is critical for ensuring quality respectful maternity care and comprehensive sexual and reproductive health. Frustrations regarding practice restrictions were expressed by professional midwives in this review, highlighting the importance of evidence-based leadership led by midwives themselves.
Essential medicines play a critical role in enabling environments for midwives. Notably, the findings indicate that midwives without mentoring did not impact the availability of medicine supplies. Weak supply chains are prevalent in LMICs, and stockouts of essential commodities pose significant barriers to delivering quality services. This underscores the essential role of mentoring or other forms of effective supportive supervision, particularly in this area [82]. The review suggests that mentoring involving managers and staff may help improve the availability of life-saving SRMNAH services. Further research is needed to identify the most effective methods for ensuring the availability of essential supplies and medicines through mentoring interventions.
The importance of data collection highlighted in the mentoring articles cannot be overstated. Midwives require effective monitoring of their performance to identify gaps and solve problems [83]. However, many countries still do not routinely use patient files, and the use of register books for storing patient information needed for macro data systems was noted. This review emphasizes the importance of effective gathering and utilization of information to ensure quality care and support at the micro-level. By highlighting gaps and facilitating feedback for improving care delivery, quality data at the micro-level is crucial.
The review found that evidence-based leadership and governance reflecting ground realities are essential. The 2018 WHO definition of Skilled Birth Attendant Standards emphasizes the importance of enabling environments [77]. The International Confederation of Midwives (ICM) defines an enabling environment for midwives as one that supports the necessary infrastructure, profession, and system-level integration for effective work performance [84]. Facility mentoring emerged as a critical factor in strengthening enabling environments and improving implementation quality [1, 53, 54]. Mentoring programs improve relationships between health system components and between staff and managers involved in care provision, aligning with the literature on addressing complex systems. Onsite facility mentoring, with frequent visits and involvement of all local authorities, integrated into all components of the related health system, proved to be the most effective approach. Further research is needed to determine best practices for mentoring approaches to inform program planners and policies that support workplace setting conducive to midwifery.
The facility mentoring findings in this review align closely with the WHO Quality Maternal Health Network guidelines, which emphasize on-site support, learning and sharing, measurement, community and stakeholder engagement, and program management as the key components for effective quality improvement in maternal health [76]. While WHO acknowledges the importance of management at the macro-level, this review highlights the criticality of on-site support for managers in facilitating sustainable change [85]. WHO may want to consider expanding its recommendations for managers to include micro-level support. The interventions evaluated in this review were further disaggregated by measures of success to deepen our understanding of known efficacy. Only a limited number of interventions assessed in-vivo changes in implementation. Self-reported changes or changes based on knowledge and skill were found to have limitations in effectively indicating implementation change, which reinforces the importance of on-site interventions [59, 60, 74, 76]. Mentoring programs should consider incorporating methods that evaluate observed implementation changes.
Mentoring programs that demonstrated positive outcomes consisted of comprehensive packages including frequent visits, capacity building, manager involvement, and strengthening of data systems. These programs consistently mentored globally standard midwives. The high-performing programs prioritized on-site capacity building activities such as group teaching, case studies, bedside teaching, assessing and advocating for supplies and equipment, establishing and reinforcing data systems, and support for problem-solving. The use of checklists for mentors was also commonly observed in many studies (Fig. 2) [49,50,51].
Several limitations of this review were identified. Firstly, the included studies exhibited diversity in their approaches, delivery methods, and outcomes, resulting in considerable heterogeneity. This heterogeneity is expected, given the inclusion of studies from different countries, diverse populations, and various public health interventions, but may lead to less accurate comparisons than a more homogeneous study. Secondly, the reliance on self-reporting of outcomes as the primary outcome method of measurement may introduce some bias, either through over- or under-reporting. Third, more nuance in terms of the most effective mentorship interventions would have given more insight, specifically the efficacy of internal versus external mentorship, but although the literature did find that frequency of mentoring contacts improved outcomes, more research is needed for more specific programmatic guidance. Finally, this review might be limited by the fact that we have employed a broad categorization for 'LMIC,' which leaves gaps in understanding specific country or region contexts.
This review highlights the importance of adhering to a global midwife definition and the role of onsite support in creating enabling environments. It identifies gaps in midwife leadership and emphasizes the need for more research to promote midwives into leadership positions. The review also underscores the significance of globally standard midwives and the challenges associated with non-standard midwives. Enabling midwives to practice to their full competencies is crucial for quality care provision leading to life saving and rights upholding, and access to essential medicine plays a critical role in creating supportive environments. Effective data collection and monitoring, as well as evidence-based leadership and governance, are essential for improving midwifery care. Onsite facility mentoring emerges as a critical component of strengthening enabling environments, and more research is needed to identify best practices for mentoring approaches.
Conclusion
Girls’ and women’s lives, and dignity depend on the availability of quality SRMNAH. To succeed in making the needed changes we need enabled, expert midwives. Midwifery literature has focused on the needed national governance and broad country understandings. There remains a need for follow up to ensure globally standard midwives are available for all girls and women. There is also a need for policy makers to include support for successful implementation. Current knowledge of health systems strengthening, and quality improvement, sheds light on the needed planning for midwives to ensure realization of their full potential. Mentoring is cost effective, and can be implemented within existing government systems. A comprehensive mentoring package inclusive of onsite capacity building of maternity staff, managers, data and procurement systems, will enable midwives to improve SRMNAH, and uphold rights for the most vulnerable.
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available due to publication restrictions from journals but are available from the corresponding author on reasonable request.
Abbreviations
- SRMNAH:
-
Sexual, reproductive, maternal, newborn and adolescent health
- LMIC:
-
Low- and middle-income country
- QI:
-
Quality improvement
- ICM:
-
International Confederation of Midwives
- SBA:
-
Skilled birth attendants
- WHO:
-
World Health Organization
References
World Health Organization. The Network for Improving Quality of Care for Maternal, Newborn and Child Health (Quality of Care Network). 2023. Available from: https://www.who.int/groups/Quality-of-care-network#:~:text=of%20Care%20Network. Accessed 1 Mar 2023.
Renfrew MJ, McFadden A, Bastos MH, Campbell J, Channon AA, Cheung NF, et al. Midwifery and quality care: findings from a new evidence-informed framework for maternal and newborn care. Lancet. 2014;384:1129–45.
Sandall J, Soltani H, Gates S, Shennan A, Devane D. Midwife-led continuity models of care compared with other models of care for women during pregnancy, birth and early parenting. Cochrane Database Syst Rev. 2016;4:CD004667.
Turkmani S, Currie S, Mungia J, Assefi N, Rahmanzai AJ, Azfar P, et al. ‘Midwives are the backbone of our health system’: lessons from Afghanistan to guide expansion of midwifery in challenging settings. Midwifery. 2013;29:1166–72.
Filby A, McConville F, Portela A. What prevents quality midwifery care? A systematic mapping of barriers in low and middle income countries from the provider perspective. PloS One. 2016;11:e0153391.
Alenchery AJ, Thoppil J, Britto CD, de Onis JV, Fernandez L, Suman Rao P. Barriers and enablers to skin-to-skin contact at birth in healthy neonates-a qualitative study. BMC Pediatrics. 2018;18:1–10.
Lencucha R, Neupane S. The use, misuse and overuse of the ‘low-income and middle-income countries’ category. BMJ Glob Health. 2022;7(6):e009067.
Starrs AM, Ezeh AC, Barker G, Basu A, Bertrand JT, Blum R, et al. Accelerate progress—sexual and reproductive health and rights for all: report of the Guttmacher-Lancet Commission. Lancet. 2018;391:2642–92.
World Health Organization. Global strategic directions for nursing and midwifery 2021-2025 2021. Available from: https://apps.who.int/iris/bitstream/handle/10665/344562/9789240033863-eng.pdf. Accessed 2 Mar 2023.
Feyissa GT, Balabanova D, Woldie M. How effective are mentoring programs for improving health worker competence and institutional performance in Africa? A systematic review of quantitative evidence. J Multidiscip Healthc. 2019;12:989–1005.
Anderson R, Zaman SB. Improving the quality of maternity care through the introduction of professional midwives and mentoring in selected sub-district hospitals in bangladesh: a mixed method study protocol. Methods Protoc. 2022;5:84.
Glickman ME, Rao SR, Schultz MR. False discovery rate control is a recommended alternative to Bonferroni-type adjustments in health studies. J Clin Epidemiol. 2014;67:850–7.
Chaturvedi S, Upadhyay S, De Costa A. Competence of birth attendants at providing emergency obstetric care under India’s JSY conditional cash transfer program for institutional delivery: an assessment using case vignettes in Madhya Pradesh province. BMC Pregnancy Childbirth. 2014;14:1–11.
UNFPA, World Health Organization & International Confederation of Midwives. The State of the World's Midwifery: A Universal Pathway. A Woman’s Right to Health 2014. Available from: https://www.unfpa.org/sites/default/files/pub-pdf/EN_SoWMy2014_complete.pdf. Accessed 2 Mar 2023.
Grant MJ, Booth A. A typology of reviews: an analysis of 14 review types and associated methodologies. Health info Libr J. 2009;26:91–108.
Anderson R, Zaman SB, Limmer M. The impact of introducing midwives and also mentoring on the quality of sexual, reproductive, maternal, newborn, and adolescent health services in low- and middle-income Countries: an integrative review protocol. Methods Protoc. 2023;6:48.
Whittemore R, Knafl K. The integrative review: updated methodology. J Adv Nurs. 2005;52:546–53.
Eldawlatly A, Alshehri H, Alqahtani A, Ahmad A, Al-Dammas F, Marzouk A. Appearance of Population, Intervention, Comparison, and Outcome as research question in the title of articles of three different anesthesia journals: a pilot study. Saudi J Anaesth. 2018;12:283.
Aromataris E, Fernandez R, Godfrey CM, Holly C, Khalil H, Tungpunkom P. Summarizing systematic reviews: methodological development, conduct and reporting of an umbrella review approach. JBI Evid Implement. 2015;13:132–40.
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Reprint—preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Phys Ther. 2009;89:873–80.
Gough D. Weight of evidence: a framework for the appraisal of the quality and relevance of evidence. Res Pap Educ. 2007;22:213–28.
Tasnim S, Rahman A, Rahman F, Kabir N, Islam F, Chowdhury S, et al. Implementing skilled midwifery services in Dhaka city urban area: Experience from community based safe motherhood project, Bangladesh. J Bangladesh Coll Phys Surg. 2011;29:10–5.
Jayanna K, Bradley J, Mony P, Cunningham T, Washington M, Bhat S, et al. Effectiveness of onsite nurse mentoring in improving quality of institutional births in the primary health centres of high priority districts of Karnataka, South India: a cluster randomized trial. PloS One. 2016;11:e0161957.
Van Lerberghe W, Matthews Z, Achadi E, Ancona C, Campbell J, Channon A, et al. Country experience with strengthening of health systems and deployment of midwives in countries with high maternal mortality. Lancet. 2014;384:1215–25.
Singh K, Brodish P, Suchindran C. A regional multilevel analysis: can skilled birth attendants uniformly decrease neonatal mortality? Matern Child Health J. 2014;18:242–9.
Vieira C, Portela A, Miller T, Coast E, Leone T, Marston C. Increasing the use of skilled health personnel where traditional birth attendants were providers of childbirth care: a systematic review. PloS One. 2012;7:e47946.
Speakman EM, Shafi A, Sondorp E, Atta N, Howard N. Development of the community midwifery education initiative and its influence on women’s health and empowerment in Afghanistan: a case study. BMC Womens Health. 2014;14:1–12.
Mumtaz Z, Levay A, Bhatti A, Salway S. Good on paper: the gap between programme theory and real-world context in Pakistan’s Community Midwife programme. BJOG. 2015;122:249–58.
Webster PC. Indonesia: the midwife and maternal mortality miasma. Can Med Assoc. 2013;185(2):E95-6.
Namazzi G, Waiswa P, Nakakeeto M, Nakibuuka VK, Namutamba S, Najjemba M, et al. Strengthening health facilities for maternal and newborn care: experiences from rural eastern Uganda. Glob Health Action. 2015;8:24271.
Fischer EA, Jayana K, Cunningham T, Washington M, Mony P, Bradley J, et al. Nurse mentors to advance quality improvement in primary health centers: lessons from a pilot program in Northern Karnataka India. Glob Health Sci Pract. 2015;3:660–75.
Bradley J, Jayanna K, Shaw S, Cunningham T, Fischer E, Mony P, et al. Improving the knowledge of labour and delivery nurses in India: a randomized controlled trial of mentoring and case sheets in primary care centres. BMC Health Serv Res. 2017;17:1–8.
Potty RS, Sinha A, Sethumadhavan R, Isac S, Washington R. Incidence, prevalence and associated factors of mother-to-child transmission of HIV, among children exposed to maternal HIV, in Belgaum district, Karnataka India. BMC Public Health. 2019;19:1–10.
Schwerdtle P, Morphet J, Hall H. A scoping review of mentorship of health personnel to improve the quality of health care in low and middle-income countries. Glob Health. 2017;13:1–8.
Tripathi S, Srivastava A, Memon P, Nair TS, Bhamare P, Singh D, et al. Quality of maternity care provided by private sector healthcare facilities in three states of India: a situational analysis. BMC Health Serv Res. 2019;19:1–9.
Manzi A, Nyirazinyoye L, Ntaganira J, Magge H, Bigirimana E, Mukanzabikeshimana L, et al. Beyond coverage: improving the quality of antenatal care delivery through integrated mentorship and quality improvement at health centers in rural Rwanda. BMC Health Serv Res. 2018;18:1–8.
Manzi A, Munyaneza F, Mujawase F, Banamwana L, Sayinzoga F, Thomson DR, et al. Assessing predictors of delayed antenatal care visits in Rwanda: a secondary analysis of Rwanda demographic and health survey 2010. BMC Pregnancy and Childbirth. 2014;14:1–8.
Tiruneh GT, Karim AM, Avan BI, Zemichael NF, Wereta TG, Wickremasinghe D, et al. The effect of implementation strength of basic emergency obstetric and newborn care (BEmONC) on facility deliveries and the met need for BEmONC at the primary health care level in Ethiopia. BMC Pregnancy Childbirth. 2018;18:1–11.
Horwood C, Haskins L, Phakathi S, McKerrow N. A health systems strengthening intervention to improve quality of care for sick and small newborn infants: results from an evaluation in district hospitals in KwaZulu-Natal South Africa. BMC Pediatr. 2019;19:1–12.
Catton HN. Developing a mentorship program in Laos. Front Public Health. 2017;5:145.
Thapa K, Dhital R, Karki YB, Rajbhandari S, Amatya S, Pande S, et al. Institutionalizing postpartum family planning and postpartum intrauterine device services in Nepal: role of training and mentorship. Int J Gynecol Obstet. 2018;143:43–8.
World Bank. Delivering the millennium development goals to reduce maternal and child mortality: a systematic review of impact evaluation evidence. 2013.
Haththotuwa R, Senanayake L, Senarath U, Attygalle D. Models of care that have reduced maternal mortality and morbidity in Sri Lanka. Int J Gynecol Obstet. 2012;119:S45–9.
Taneja G, Sarin E, Bajpayee D, Chaudhuri S, Verma G, Parashar R, et al. Care around birth approach: a training, mentoring, and quality improvement model to optimize intrapartum and immediate postpartum quality of care in India. Glob Health Sci Pract. 2021;9:590–610.
Barnhart DA, Spiegelman D, Zigler CM, Kara N, Delaney MM, Kalita T, et al. Coaching intensity, adherence to essential birth practices, and health outcomes in the BetterBirth Trial in Uttar Pradesh India. Glob Health Sci Pract. 2020;8:38–54.
Geldsetzer P, Mboggo E, Larson E, Lema IA, Magesa L, Machumi L, et al. Community health workers to improve uptake of maternal healthcare services: a cluster-randomized pragmatic trial in Dar es Salaam Tanzania. PLoS Med. 2019;16:e1002768.
Ngabonzima A, Kenyon C, Hategeka C, Utuza AJ, Banguti PR, Luginaah I, et al. Developing and implementing a novel mentorship model (4+ 1) for maternal, newborn and child health in Rwanda. BMC Health Serv Res. 2020;20:1–11.
Ngabonzima A, Kenyon C, Kpienbaareh D, Luginaah I, Mukunde G, Hategeka C, et al. Developing and implementing a model of equitable distribution of mentorship in districts with spatial inequities and maldistribution of human resources for maternal and newborn care in Rwanda. BMC Health Serv Res. 2021;21:1–12.
Haskins L, Chiliza J, Barker P, Connolly C, Phakathi S, Feeley A, et al. Evaluation of the effectiveness of a quality improvement intervention to support integration of maternal, child and HIV care in primary health care facilities in South Africa. BMC Public Health. 2020;20:1–12.
Stephens B, Mwandalima IJ, Samma A, Lyatuu J, Mimno K, Komwihangiro J. Reducing barriers to postabortion contraception: the role of expanding coverage of postabortion care in Dar es Salaam Tanzania. Glob Health Sci Pract. 2019;7:S258–70.
Marx Delaney M, Kalita T, Hawrusik B, Neal B, Miller K, Ketchum R, et al. Modification of oxytocin use through a coaching-based intervention based on the WHO Safe Childbirth Checklist in Uttar Pradesh, India: a secondary analysis of a cluster randomised controlled trial. BJOG. 2021;128:2013–21.
Magge H, Nahimana E, Mugunga JC, Nkikabahizi F, Tadiri E, Sayinzoga F, et al. The all babies count initiative: impact of a health system improvement approach on neonatal care and outcomes in Rwanda. Glob Health Sci Pract. 2020;8:000.
Hoover J, Koon AD, Rosser EN, Rao KD. Mentoring the working nurse: a scoping review. Hum Resour Health. 2020;18:1–10.
McFadden A, Gupta S, Marshall JL, Shinwell S, Sharma B, McConville F, et al. Systematic review of barriers to, and facilitators of, the provision of high-quality midwifery services in India. Birth. 2020;47:304–21.
Rao KD, Srivastava S, Warren N, Mayra K, Gore A, Das A, et al. Where there is no nurse: an observational study of large-scale mentoring of auxiliary nurses to improve quality of care during childbirth at primary health centres in India. BMJ Open. 2019;9:e027147.
Waiswa P, Wanduru P, Okuga M, Kajjo D, Kwesiga D, Kalungi J, et al. Institutionalizing a regional model for improving quality of newborn care at birth across hospitals in eastern Uganda: a 4-year story. Glob Health Sci Pract. 2021;9:365–78.
Oosthuizen SJ, Bergh A-M, Grimbeek J, Pattinson RC. Midwife-led obstetric units working ‘CLEVER’: Improving perinatal outcome indicators in a South African health district. S Afr Med J. 2019;109:95–101.
Feeley C, Crossland N, Betran AP, Weeks A, Downe S, Kingdon C. Training and expertise in undertaking assisted vaginal delivery (AVD): a mixed methods systematic review of practitioners views and experiences. Reprod Health. 2021;18:1–22.
Michel-Schuldt M, McFadden A, Renfrew M, Homer C. The provision of midwife-led care in low-and middle-income countries: an integrative review. Midwifery. 2020;84:102659.
Anderson R, Williams A, Jess N, Read JM, Limmer M. The impact of professional midwives and mentoring on the quality and availability of maternity care in government sub-district hospitals in Bangladesh: a mixed-methods observational study. BMC Pregnancy Childbirth. 2022;22:827.
Bogren M, Begum F, Erlandsson K. The historical development of the midwifery profession in Bangladesh. J Asian Midwives (JAM). 2017;4:65–74.
Bogren MU, van Teijlingen E, Berg M. Where midwives are not yet recognised: a feasibility study of professional midwives in Nepal. Midwifery. 2013;29:1103–9.
ten Hoope-Bender P, de Bernis L, Campbell J, Downe S, Fauveau V, Fogstad H, et al. Improvement of maternal and newborn health through midwifery. Lancet. 2014;384:1226–35.
Save the children and UNFPA. Brief: Integration of Midwifery Services into the Health System 2021. Available from: https://bangladesh.savethechildren.net/sites/bangladesh.savethechildren.net/files/library/SNMP%20Brief_Final_080221_1.pdf. Accessed 2 Mar 2023.
Erlandsson K, Doraiswamy S, Wallin L, Bogren M. Capacity building of midwifery faculty to implement a 3-years midwifery diploma curriculum in Bangladesh: a process evaluation of a mentorship programme. Nurse Educ Pract. 2018;29:212–8.
Bogren M, Erlandsson K, Byrskog U. What prevents midwifery quality care in Bangladesh? A focus group enquiry with midwifery students. BMC Health Serv Res. 2018;18:1–9.
Bartlett L, Weissman E, Gubin R, Patton-Molitors R, Friberg IK. The impact and cost of scaling up midwifery and obstetrics in 58 low-and middle-income countries. PloS One. 2014;9:e98550.
Dawson A, Nkowane A, Whelan A. Approaches to improving the contribution of the nursing and midwifery workforce to increasing universal access to primary health care for vulnerable populations: a systematic review. Hum Resour Health. 2015;13:1–23.
Namazzi G, Achola KA, Jenny A, Santos N, Butrick E, Otieno P, et al. Implementing an intrapartum package of interventions to improve quality of care to reduce the burden of preterm birth in Kenya and Uganda. Implement Sci commun. 2021;2:1–13.
Sangy MT, Duaso M, Feeley C, Walker S. Barriers and facilitators to the implementation of midwife-led care for childbearing women in low- and middle-income countries: a mixed-methods systematic review. Midwifery. 2023;122:103696.
Mwansisya T, Mbekenga C, Isangula K, Mwasha L, Mbelwa S, Lyimo M, et al. The impact of training on self-reported performance in reproductive, maternal, and newborn health service delivery among healthcare workers in Tanzania: a baseline-and endline-survey. Reprod Health. 2022;19:143.
Pappu NI, Öberg I, Byrskog U, Raha P, Moni R, Akhtar S, et al. The commitment to a midwifery centre care model in Bangladesh: An interview study with midwives, educators and students. PloS One. 2023;18: e0271867.
Brac University. Developing midwives: ten years of learning 2022. Accessed on 11 Feb 2023. Available from: https://bracjpgsph.org/assets/pdf/dmp/events/DEVELOPING%20MIDWIVES-TEN%20YEARS%20OF%20LEARNING_compressed.pdf.
Anderson R, Williams A, Emdadul Hoque DM, Jess N, Shahjahan F, Hossain A, et al. Implementing midwifery services in public tertiary medical college hospitals in Bangladesh: a longitudinal study. Women Birth. 2023;36(3):299–304.
Kieny M-P, Evans TG, Scarpetta S, Kelley ET, Klazinga N, Forde I, et al. Delivering quality health services: a global imperative for universal health coverage. Washington, DC: World Bank Group; 2018.
World Health Organization. Five functions to improve quality of care for maternal newborn and child health: knowledge brief 2021. Accessed on 27 May 2023. Available from: https://apps.who.int/iris/bitstream/handle/10665/350118/9789240039025-eng.pdf.
World Health Organization. Definition of skilled health personnel providing care during childbirth: the 2018 joint statement by WHO, UNFPA, UNICEF, ICM, ICN, FIGO and IPA: World Health Organization; 2018. Accessed on 28 May 2023. Available from: https://apps.who.int/iris/bitstream/handle/10665/272818/WHO-RHR-18.14-eng.pdf?ua=1.
Elliott S, Murrell K, Harper P, Stephens T, Pellowe C. A comprehensive systematic review of the use of simulation in the continuing education and training of qualified medical, nursing and midwifery staff. JBI Evid Synth. 2011;9:538–87.
Chowdhury R, Sinha B, Sankar MJ, Taneja S, Bhandari N, Rollins N, et al. Breastfeeding and maternal health outcomes: a systematic review and meta-analysis. Acta Paediatr. 2015;104:96–113.
Hewitt L, Dahlen HG, Hartz DL, Dadich A. Leadership and management in midwifery-led continuity of care models: a thematic and lexical analysis of a scoping review. Midwifery. 2021;98:102986.
Ten Hoope Bender P, Homer C, Matthews Z, Nove A, Sochas L, Campbell J, et al. The state of the world’s midwifery: a universal pathway, a woman’s right to health. 2014.
Bailey P, Paxton A, Lobis S, Fry D. The availability of life-saving obstetric services in developing countries: an in-depth look at the signal functions for emergency obstetric care. Int J Gynecol Obstet. 2006;93:285–91.
Ndabarora E, Chipps JA, Uys L. Systematic review of health data quality management and best practices at community and district levels in LMIC. Info Dev. 2014;30:103–20.
International Confederation of Midwives. Essential Competencies for Midwifery Practice, 2019 update 2019. Accessed on 11 Feb 2023. Available from: https://www.internationalmidwives.org/assets/files/general-files/2019/10/icm-competencies-en-print-october-2019_final_18-oct-5db05248843e8.pdf.
Reed JE, Green S, Howe C. Translating evidence in complex systems: a comparative review of implementation and improvement frameworks. Int J Qual Health Care. 2019;31:173–82.
Acknowledgements
Not applicable.
Funding
This research received no external funding.
Author information
Authors and Affiliations
Contributions
RA conceived the design of this systematic review and drafted the first version of the manuscript. SBZ, ANJ, JMR, and ML has contributed substantially, providing inputs to the manuscript and revising it critically. All authors have reviewed and agreed to the submitted version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Anderson, R., Zaman, S.B., Jimmy, A.N. et al. Strengthening quality in sexual, reproductive, maternal, and newborn health systems in low- and middle-income countries through midwives and facility mentoring: an integrative review. BMC Pregnancy Childbirth 23, 712 (2023). https://0-doi-org.brum.beds.ac.uk/10.1186/s12884-023-06027-0
Received:
Accepted:
Published:
DOI: https://0-doi-org.brum.beds.ac.uk/10.1186/s12884-023-06027-0